Surgery today is safer than ever before – not because risks have disappeared, but because hospitals and surgical centers follow strict, science-based systems to control them. Patient safety in surgery is no longer just a goal; it is the foundation of every modern medical practice.
At Shenandoah Valley Surgical Associates (SVSA) in Fishersville, Virginia, this commitment to safety guides every decision, from the moment a patient schedules a procedure to full recovery. The entire team surgeons, anesthesiologists, nurses, and technologists works together to prevent complications, infections, and communication errors.
Whether a patient undergoes a complex vascular intervention or a simple outpatient procedure, the same protocols apply: meticulous planning, sterile technique, careful monitoring, and continuous communication. SVSA’s mission is to deliver quality care in Fishersville that meets or exceeds all national and international safety standards.
Safety, however, is not achieved by technology alone. It depends on teamwork, transparency, and an unbroken chain of accountability. Every person in the operating room — from the scrub nurse to the lead surgeon — has the authority to speak up if something doesn’t seem right. That philosophy of shared vigilance is what keeps patients safe.
National Standards for Surgical Safety
The framework for patient safety in surgery has been built over decades of research and experience. Global and national healthcare organizations including the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and the Society for Vascular Surgery (SVS) — have established proven systems to minimize risk, prevent infection, and improve outcomes. SVSA incorporates each of these best practices into its daily operations.
WHO Surgical Safety Checklist
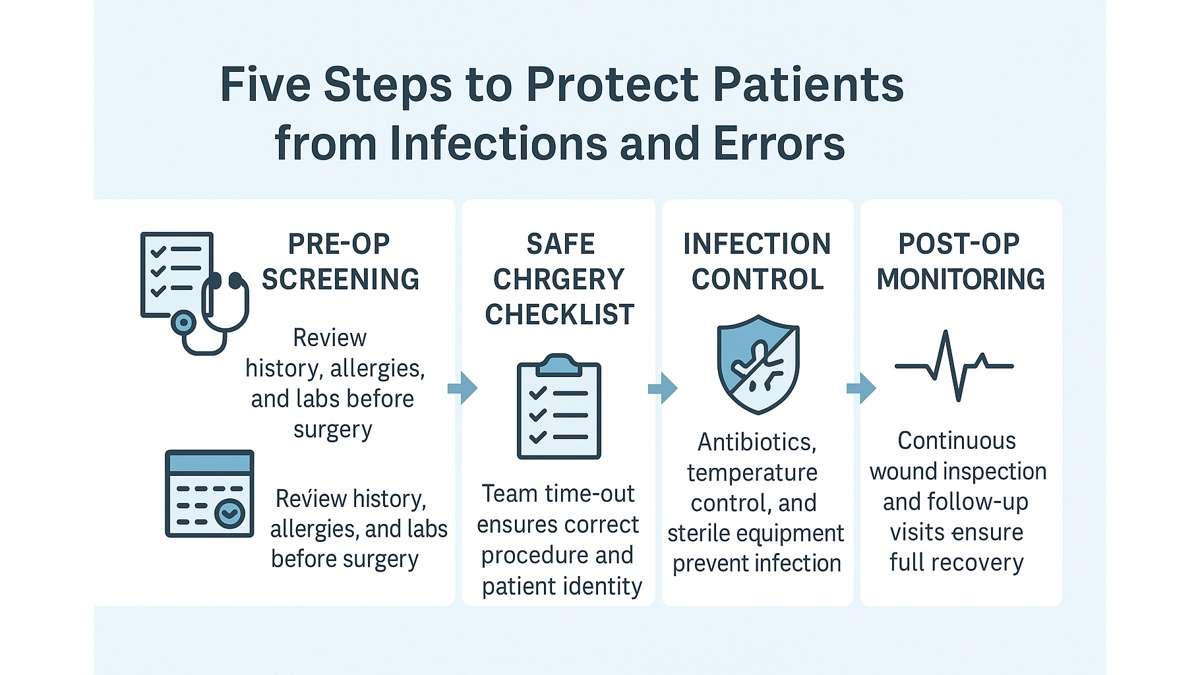
The World Health Organization’s Surgical Safety Checklist is one of the most important tools in modern surgery. It consists of 19 key steps performed at three critical stages before anesthesia, before incision, and before leaving the operating room.
At SVSA, this checklist is applied to every case, no matter how small. The team confirms:
- the patient’s full identity and procedure details;
- the exact surgical site and side (right or left limb, artery, etc.);
- known allergies, medical conditions, and anesthesia risks;
- availability of critical instruments, implants, and imaging;
- postoperative plans, including antibiotic and pain management protocols.
This “pause for safety” known as a surgical time-out ensures that everyone in the room agrees on what will be done. It prevents errors such as wrong-site surgery, incorrect equipment use, or omitted safety steps.
Since its introduction, the WHO checklist has reduced complications and deaths related to surgery by up to 30%, according to multiple global studies. It is now considered the gold standard for surgical team communication and accountability.
CDC Guidelines for Infection Control
Infections are one of the most preventable complications in surgical care. The Centers for Disease Control and Prevention (CDC) sets national standards for infection control that focus on patient preparation, antibiotic timing, and sterile technique. SVSA integrates these recommendations into every stage of the surgical process.
Key elements include:
- Preoperative skin preparation: antiseptic cleansing of the surgical site to reduce bacteria.
- Antibiotic prophylaxis: administering the correct antibiotic within 60 minutes before incision.
- Temperature and glucose control: maintaining normal body temperature and blood sugar levels during surgery to aid healing.
- Strict sterile protocols: single-use drapes, sterilized instruments, and limited room traffic during procedures.
After surgery, wound care instructions are clearly explained to every patient, and follow-up appointments ensure that healing progresses without infection.
This proactive, data-driven approach keeps postoperative infection rates at SVSA well below the national average.
Society for Vascular Surgery (SVS) – Quality and Safety Programs
As a vascular and general surgery practice, SVSA participates in the Vascular Quality Initiative (VQI) a nationwide program led by the Society for Vascular Surgery. This program collects data from hospitals across the United States to track patient outcomes, identify trends, and continuously improve standards of care.
By benchmarking its results against national data, SVSA can measure its performance in key areas such as infection prevention, complication rates, and readmissions. The VQI system allows immediate feedback and helps implement evidence-based improvements to keep patients safer.
The result is continuous progress each case contributes to better care for the next patient.
Accreditation and Oversight
Safety also depends on regulation and transparency. SVSA’s facilities comply with standards established by the Joint Commission and the Centers for Medicare & Medicaid Services (CMS). These agencies regularly inspect surgical centers to verify compliance with national requirements on equipment sterilization, patient privacy, and emergency readiness.
This oversight ensures that every SVSA patient is treated in an environment that meets the same rigorous safety benchmarks as major academic hospitals.
Safety as a Shared Responsibility
Ultimately, even the best systems are only as strong as the people who use them. SVSA fosters a safety-first culture where every staff member is encouraged to voice concerns. If a nurse, technician, or anesthesiologist notices a potential problem whether it’s a mislabeled sample or an equipment issue — they have full authority to stop the procedure until it is resolved.
This collective accountability creates a work environment where vigilance is the norm, not the exception. It also reassures patients that their care is delivered by a team fully united in purpose: to protect their health and safety above all else.
How SVSA Ensures Sterility and Infection Control
Preventing infection is one of the most important aspects of patient safety in surgery. Even the smallest lapse in sterilization can lead to postoperative complications. For this reason, Shenandoah Valley Surgical Associates (SVSA) maintains an uncompromising infection-control protocol that aligns with CDC and WHO standards.
Surgical Environment
SVSA’s operating suites are designed with positive-pressure ventilation systems that continuously filter and circulate clean air, reducing airborne particles and microorganisms. Temperature and humidity are monitored electronically to maintain conditions that inhibit bacterial growth.
Before each day’s first case, and between every procedure, every surface, instrument table, and monitor is disinfected using hospital-grade solutions approved by the Environmental Protection Agency (EPA). Disposable drapes and covers are used wherever possible to eliminate cross-contamination.
Instrument Sterilization
All surgical instruments undergo a multi-stage cleaning process:
- Ultrasonic cleaning to remove microscopic debris.
- Steam autoclaving under high pressure and temperature.
- Chemical indicator verification to confirm sterilization integrity.
Each tray is sealed, labeled, and logged in SVSA’s electronic tracking system, ensuring full traceability. Sterility audits are performed weekly by the infection-control officer.
Antibiotic Stewardship
The correct use of antibiotics is vital to prevent resistance and infections. SVSA follows CDC timing guidelines, administering prophylactic antibiotics within 60 minutes before incision and discontinuing them within 24 hours after surgery unless otherwise required. This evidence-based approach minimizes both infection risk and unnecessary antibiotic exposure.
Staff Hygiene and Training
Every staff member completes mandatory hand-hygiene training and competency checks twice per year. Alcohol-based sanitizers are placed at every room entry and exit. During procedures, the team follows the “scrub in, glove up, mask on” protocol verified by a circulating nurse before the operation begins.
In addition, SVSA holds regular “infection-control drills,” during which scenarios such as equipment contamination or a break in sterile field are simulated. These exercises help maintain quick, coordinated responses.
Patient Preparation
Infection control starts before the incision. Patients are instructed to shower with antiseptic soap the night before surgery, avoid shaving the surgical site, and wear clean, loose-fitting clothing on the day of the procedure. For vascular cases, the skin is prepped with chlorhexidine solution, and sterile drapes isolate the area throughout the operation.
Postoperatively, patients receive clear written and verbal wound-care instructions to ensure that sterility is maintained at home.
Multi-Level Equipment and Staff Safety Checks
Beyond infection control, multi-tiered verification systems ensure that every procedure at SVSA runs safely and smoothly from start to finish.
The Surgical Checklist
Before every operation, the team performs a three-phase safety pause based on the WHO checklist:
- Sign-In (before anesthesia): verifies patient identity, consent, allergies, and equipment readiness.
- Time-Out (before incision): confirms procedure, site, and special considerations; all members verbally agree.
- Sign-Out (before leaving OR): counts instruments, confirms specimen labeling, reviews postoperative plans.
This routine may seem repetitive, but studies show it prevents wrong-site surgery, lost instruments, and miscommunication.
Equipment Calibration and Maintenance
Every surgical and endovascular device angiography systems, imaging monitors, cautery units, and anesthesia machines — is calibrated on a scheduled basis. Biomedical engineers test alarms, backup batteries, and pressure sensors before each day’s first case.
Disposable catheters, guidewires, and stents are inspected for integrity and expiration before use. Any item that fails inspection is immediately replaced and reported through SVSA’s equipment-safety tracking platform.
Staff Credentialing and Competency
All surgeons at SVSA are board-certified and maintain FACS (Fellow of the American College of Surgeons) status, reflecting ongoing education and adherence to professional standards. Nurses and technologists complete yearly competency assessments covering sterile technique, radiation safety, and emergency response.
This rigorous credentialing process ensures that every individual in the operating room meets national standards for training and safety performance.
Communication and Cross-Verification
To minimize human error, SVSA employs “dual confirmation” for all critical steps: blood type verification, implant selection, and medication dosing. Two team members must verbally confirm before proceeding. This collaborative approach supports redundancy — a fundamental principle of quality care and Fishersville surgical safety.
Stage of Surgery / Safety Measures
| Stage of Surgery | Safety Measures Implemented |
|---|---|
| Pre-operative Preparation | Sterile instrument checks, surgical-site marking, patient identity and allergy verification |
| Intra-operative (During Surgery) | WHO Safety Checklist, sterile draping, continuous monitoring of vitals and equipment alarms |
| Post-operative Phase | Timed antibiotic prophylaxis, wound-care education, infection-control surveillance, temperature and glucose stabilization |
This table summarizes SVSA’s comprehensive, step-by-step commitment to safety at every stage of the surgical process.
How Patients Can Participate in Their Own Safety
While hospitals and surgical centers implement robust safety systems, the patient also plays a key role in maintaining a safe environment. Patient involvement is one of the most effective ways to prevent errors and improve outcomes. At Shenandoah Valley Surgical Associates (SVSA), patients are encouraged to be active partners in their care.
Ask Questions and Understand Your Procedure
Before your operation, don’t hesitate to ask your surgeon to explain what will happen, why it’s needed, and what results to expect. Understanding your procedure reduces anxiety and helps you recognize anything that seems unfamiliar.
Questions you can ask include:
- What type of anesthesia will I receive?
- How long will recovery take?
- What are the possible side effects or complications?
Clear communication ensures alignment between your expectations and your surgical plan a cornerstone of quality care in Fishersville.
Keep an Updated List of Medications
Provide your surgeon and anesthesiologist with a detailed list of all medications, supplements, and over-the-counter drugs you use. This helps prevent dangerous interactions, especially with blood thinners or diabetes medications.
Follow Preoperative and Postoperative Instructions Exactly
Every instruction you receive from not eating before anesthesia to keeping your wound dry is based on safety evidence. Ignoring or forgetting these details increases risk. If something is unclear, call your care team to clarify. SVSA nurses are available to guide patients through every step.
Practice Good Hygiene
Take an antiseptic shower before your surgery, wear clean clothes, and avoid shaving the surgical area to reduce skin irritation and bacterial spread. After surgery, wash your hands before touching your incision or dressing.
Speak Up About Concerns
If you notice that a caregiver hasn’t washed their hands or if you spot something that seems incorrect – say so. Patient advocacy is supported and encouraged at SVSA. Every team member is trained to respond positively when a patient raises a safety concern.
Involve Family or a Care Partner
Having a trusted person with you during preoperative discussions helps ensure that instructions are remembered correctly. Family members can also help monitor recovery and communicate with the care team after discharge.
By staying engaged, patients contribute directly to their own protection and recovery success. Safe care is always a shared responsibility between providers and patients.
Frequently Asked Questions (FAQ)
What safety measures are taken before surgery?
Your identity, procedure type, and surgical site are verified multiple times. Equipment and instruments are sterilized and checked before each case.
What is a surgical checklist?
It’s a structured list developed by the WHO to confirm all safety steps before, during, and after surgery. Every SVSA procedure follows it.
How are infections prevented?
Through antibiotic timing, sterile technique, hand hygiene, and environmental controls such as filtered airflow and temperature regulation.
Can a family member be present before surgery?
Yes. Family members are welcome before anesthesia and after surgery in recovery areas to support patient comfort.
Author:
Dr. Charles D. Goff, MD, FACS

Sources
World Health Organization — Safe Surgery: Tool and Resources (Surgical Safety Checklist)
Centers for Disease Control and Prevention — Surgical Site Infection (SSI) Prevention
WHO / Global Guidelines — Guidelines for the Safe Surgery and Surgical Safety Checklist — NCBI
Agency for Healthcare Research and Quality (AHRQ) — Implementing the Surgical Safety Checklist — ahrq.gov