Many people mistake early signs of vascular disease for ordinary fatigue, aging, or muscle pain. Yet what seems like a mild discomfort can signal a deeper problem with circulation – one that may progress quietly until it becomes serious.
Knowing when to see a vascular specialist is essential for maintaining healthy blood flow throughout the body. Problems with arteries and veins can affect the legs, brain, kidneys, and even the heart. The sooner they are detected, the easier they are to treat without major surgery.
If you’ve ever searched online for a vascular surgeon near me, you’ve already taken an important step toward protecting your long-term health. This guide will help you recognize warning signs, understand what a vascular surgeon does, and know what to expect during your first consultation at Shenandoah Valley Surgical Associates (SVSA) in Fishersville, Virginia.
Common Symptoms of Vascular Disorders
Vascular conditions often develop gradually, giving only subtle clues at first. However, the body tends to send clear signals when circulation begins to fail. Recognizing these poor circulation symptoms can help you act before irreversible damage occurs.
Leg Pain or Cramping When Walking
Pain, tightness, or cramping in the calves, thighs, or hips while walking which improves after rest is called claudication. It’s a classic symptom of peripheral artery disease (PAD), caused by narrowing of the arteries that supply the legs.
Numbness or Coldness in the Feet
If one leg or foot feels consistently colder or more numb than the other, circulation could be impaired. Reduced blood flow means the tissues are not getting enough oxygen, which can lead to sores or ulcers that heal slowly.
Skin Discoloration or Hair Loss on the Legs
Bluish or dark patches, shiny skin, or loss of leg hair can all be early signs of vascular disease. When the skin’s oxygen supply decreases, its appearance changes — sometimes long before pain begins.
Swelling or Bulging Veins
Swollen, twisted veins in the legs may indicate varicose veins or chronic venous insufficiency, where the valves inside the veins don’t close properly. Although not always dangerous, untreated venous problems can cause leg heaviness, fatigue, and ulcers over time.
Dizziness, Vision Changes, or Facial Numbness
These symptoms can be linked to carotid artery disease, a narrowing of the arteries that carry blood to the brain. Blockage in these vessels increases the risk of stroke, especially when accompanied by transient weakness or speech difficulty.
Non-Healing Wounds on the Feet or Toes
Poor circulation slows the healing process. Small cuts or sores that persist for weeks, particularly in people with diabetes, can become infected or lead to tissue loss (gangrene) if not treated promptly.
Pain at Rest
When blood flow becomes severely restricted, pain may appear even when you are not walking. Nighttime foot pain that improves when the leg is dangled off the bed is a red flag for advanced vascular disease.
If you experience any of these symptoms, it’s important to schedule an evaluation as soon as possible. Many conditions can be treated effectively without major surgery if caught early.
Why You Shouldn’t Delay a Vascular Evaluation
Ignoring circulation issues can lead to complications that are far more difficult to manage later. Modern vascular care is highly effective — but timing is everything.
Early Detection Prevents Major Complications
Conditions like peripheral artery disease, carotid stenosis, and venous insufficiency progress silently. By the time symptoms become severe, arteries or veins may already be significantly blocked. Early diagnosis through simple tests such as ABI (ankle-brachial index) or ultrasound can identify problems before they threaten limb or organ function.
Vascular Health Affects the Whole Body
The vascular system is the body’s delivery network. When circulation fails in one area, it can signal broader issues – including an increased risk of heart attack and stroke. Research from the Centers for Disease Control and Prevention (CDC) shows that vascular disease shares risk factors with coronary artery disease, such as smoking, high blood pressure, diabetes, and elevated cholesterol.
Minimally Invasive Treatments Work Best Early
Modern vascular specialists use catheter-based procedures and imaging-guided techniques to restore blood flow. These approaches are most effective when disease is detected early, before arteries become completely blocked or tissue damage occurs.
Delaying Care Can Lead to Limb Loss
Advanced peripheral artery disease can result in critical limb ischemia, where blood flow is so poor that the tissue begins to die. In severe cases, amputation becomes necessary. Early screening and intervention can prevent this outcome in nearly all patients.
Peace of Mind Through Professional Evaluation
Even if your symptoms are mild or intermittent, consulting a specialist offers clarity. Noninvasive tests can quickly confirm whether circulation is normal. For many patients, this peace of mind is as valuable as treatment itself.
If you’ve noticed pain, swelling, numbness, or discoloration in your legs, don’t ignore it. Schedule an appointment with a vascular surgeon near me to understand your vascular health and explore treatment options before problems progress.
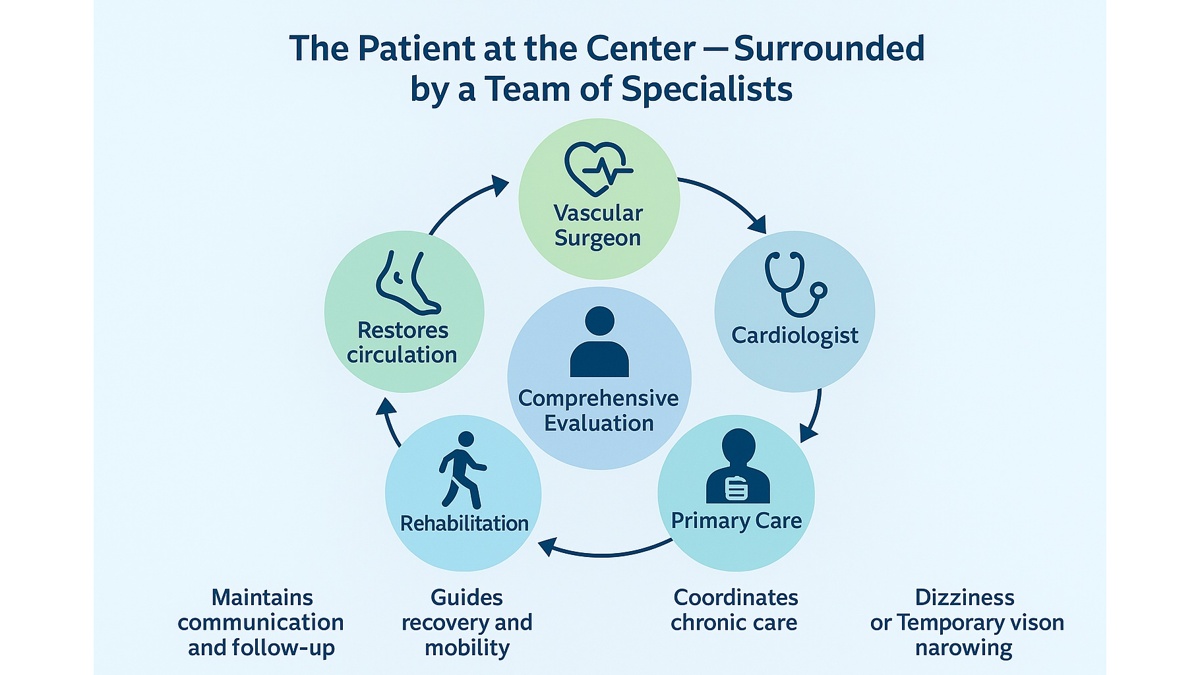
How Vascular Surgeons, Primary Care Physicians, and Cardiologists Collaborate
The foundation of effective multidisciplinary care lies in seamless communication between specialists. At Shenandoah Valley Surgical Associates (SVSA), every patient’s journey involves collaboration between vascular surgeons, general surgeons, primary care physicians, cardiologists, and rehabilitation experts. Each plays a distinct but interconnected role in maintaining circulation, organ function, and overall wellness.
The Vascular Surgeon: Restoring Circulation
A vascular surgeon’s primary focus is on the arteries and veins — the body’s vital transportation network. Using both traditional and minimally invasive procedures, they repair blockages, improve blood flow, and prevent complications such as stroke or limb ischemia. However, their role extends beyond surgery. They rely on input from cardiologists and internists to evaluate a patient’s cardiovascular status before and after an operation.
The Primary Care Physician: Monitoring the Whole Picture
The primary care physician (PCP) is often the first to notice symptoms like leg pain, swelling, or dizziness. They coordinate diagnostic screenings, manage chronic conditions such as hypertension or diabetes, and communicate directly with surgical specialists when needed. At SVSA, PCPs remain involved throughout the entire process, ensuring that general health and medication management support the surgical plan.
The Cardiologist: Protecting the Heart During Vascular Treatment
Because vascular disease and heart disease share the same risk factors, cardiologists play a key role in preoperative evaluation. They ensure that the patient’s heart can tolerate anesthesia or vascular procedures. They also manage long-term medications such as statins and antiplatelet therapy. In turn, vascular surgeons provide feedback about how improved circulation affects heart workload, closing the loop between specialties.
The Rehabilitation Specialist: Helping Recovery and Mobility
After surgery or intervention, rehabilitation experts create custom exercise programs to strengthen muscles and restore walking ability. Early movement reduces the risk of clot formation and helps maintain long-term circulation. At SVSA, rehab specialists receive updates directly from surgeons, ensuring that recovery plans align with the patient’s healing stage.
The Nursing and Care Coordination Team
Nurses and care coordinators bridge communication between the patient and the entire multidisciplinary team. They track progress, schedule follow-up visits, and ensure that every professional has access to updated clinical notes. This system prevents confusion and guarantees that the patient’s treatment plan remains cohesive.
Together, these professionals form the vascular and general surgery team that defines SVSA’s integrated care model — one where every decision is discussed, refined, and implemented collaboratively.
How Patients Benefit from Coordinated Care
For patients, multidisciplinary care translates into more than just convenience — it can directly improve survival, recovery time, and overall quality of life.
Faster, More Accurate Diagnosis
When multiple specialists assess a case simultaneously, diagnosis is faster and more precise. For instance, leg pain might be misattributed to joint disease or neuropathy, but collaboration between a PCP, vascular surgeon, and radiologist can quickly identify it as peripheral artery disease (PAD).
Safer Surgery and Recovery
Preoperative clearance by cardiology, combined with detailed imaging from vascular specialists, reduces surgical risk. Continuous monitoring by primary care physicians postoperatively ensures medication safety and early detection of complications.
Personalized, Continuous Care
Instead of fragmented consultations, patients experience continuity from the first visit through recovery and follow-up. SVSA maintains detailed electronic medical records accessible to all participating specialists, ensuring consistent treatment decisions.
Reduced Stress and Confusion
Coordinated care eliminates the need for patients to relay information between doctors. A single, unified plan provides reassurance that everyone on the team is aware of the patient’s condition and progress.
Long-Term Prevention
Once treatment is complete, patients continue receiving preventive care. The team educates them about exercise, smoking cessation, and diet modification. This ongoing collaboration helps prevent disease recurrence and supports long-term vascular health.
Table: Specialist — Role — Example of Collaboration
| Specialist | Role in Care | Example of Collaboration |
|---|---|---|
| Vascular Surgeon | Diagnosis and treatment of vessel disease | Performs bypass or stenting while coordinating with cardiologist for cardiac safety |
| Primary Care Physician | Oversees overall health and chronic conditions | Adjusts medications pre- and post-surgery to optimize healing |
| Cardiologist | Manages heart function and blood pressure | Evaluates risk before vascular surgery and monitors recovery |
| Rehabilitation Specialist | Restores mobility and function | Designs exercise program after vascular repair |
| Nurse / Care Coordinator | Tracks communication and follow-up | Ensures all test results and updates reach each specialist |
This table reflects how each professional contributes unique expertise to a patient-centered treatment plan.
Example of a Patient’s Journey at SVSA
At Shenandoah Valley Surgical Associates (SVSA) in Fishersville, Virginia, every patient receives coordinated, team-based care. The process is structured, transparent, and designed to ensure that no detail is overlooked. Below is an example of how this multidisciplinary care in Virginia works in real practice.
Step 1: Referral or Self-Initiated Consultation
A patient notices leg pain when walking or persistent swelling and schedules an appointment sometimes through their primary care provider, sometimes directly with SVSA. The clinic’s staff collects prior medical records and imaging to provide a full background for the care team.
Step 2: Comprehensive Evaluation
During the first visit, a vascular and general surgery team reviews the patient’s history, symptoms, and risk factors. Diagnostic tests such as ultrasound or ankle-brachial index (ABI) are performed on-site. If heart or blood pressure issues are identified, a cardiologist is immediately included in the case.
Step 3: Multidisciplinary Case Review
Within the same week, the vascular surgeon discusses findings with the cardiologist and primary care physician. Together they determine the safest and most effective plan — whether that’s medication management, minimally invasive stenting, or surgical intervention. This team review ensures consistency: one plan, one message, and one goal for every provider involved.
Step 4: Treatment and Coordination
If a procedure is needed, the same team coordinates all aspects — from scheduling and preoperative testing to post-operative recovery. Communication continues in real time through shared records and direct messaging between offices. The patient never has to “relay” updates; it’s all handled internally.
Step 5: Recovery and Rehabilitation
After treatment, rehabilitation specialists develop personalized activity plans to restore strength and circulation. The vascular surgeon and primary care provider track healing progress, while the cardiologist adjusts medications to support optimal recovery. Because everyone has access to the same data, any complication can be detected early and managed promptly.
Step 6: Long-Term Prevention
When recovery is complete, SVSA emphasizes prevention. Lifestyle coaching, blood pressure control, and regular vascular screenings become part of the ongoing plan. Patients stay in touch with the same integrated network, ensuring continuous protection of their vascular health.
This coordinated system turns what could be a stressful, fragmented medical experience into a guided, team-supported journey. It’s a model of integrated healthcare that SVSA applies to every patient — not just for treatment, but for lifelong wellness.
Frequently Asked Questions (FAQ)
Why is team-based treatment important?
It combines the expertise of multiple specialists, ensuring every aspect of your health is addressed.
How many doctors are involved in my case?
Typically three to five — including a vascular surgeon, primary care physician, and cardiologist, depending on your condition.
Who coordinates the process?
SVSA’s care coordination team manages scheduling, communication, and updates between all specialists.
Can I get a second opinion?
Yes. Patients are encouraged to seek second opinions, and SVSA can share diagnostic results securely with other providers.
How does SVSA work with my family doctor?
Your family doctor remains part of the care team, receiving full reports and updates to ensure continuity.
Call to Action (CTA)
At SVSA, your health is never managed by one specialist alone — it’s guided by an entire team. Our vascular and general surgery team collaborates with cardiologists, internists, and rehabilitation experts to create a treatment plan designed just for you. Experience how multidisciplinary care in Virginia can make every step of your recovery safer, faster, and more effective.
Author:
William G. Thompson

Sources
- The Impact of Interdisciplinary Team-Based Care on the Care and Outcomes of Patients – R Kongkar et al., 2025. PMC article
- Multidisciplinary care in surgery: Are team-based interventions cost-effective? – M J Davis et al., 2021. PubMed article
- Innovative health and social integrated care model: effects on chronic patient quality of life – E Gavaldà-Espelta et al., 2023. PMC article
- Integrated care interventions involving primary care: effects on primary care functions and outcomes – Y Zhang et al., 2025. BMC Health Policy & Systems
- Multidisciplinary teams working for integrated care – SCIE resource (United Kingdom)