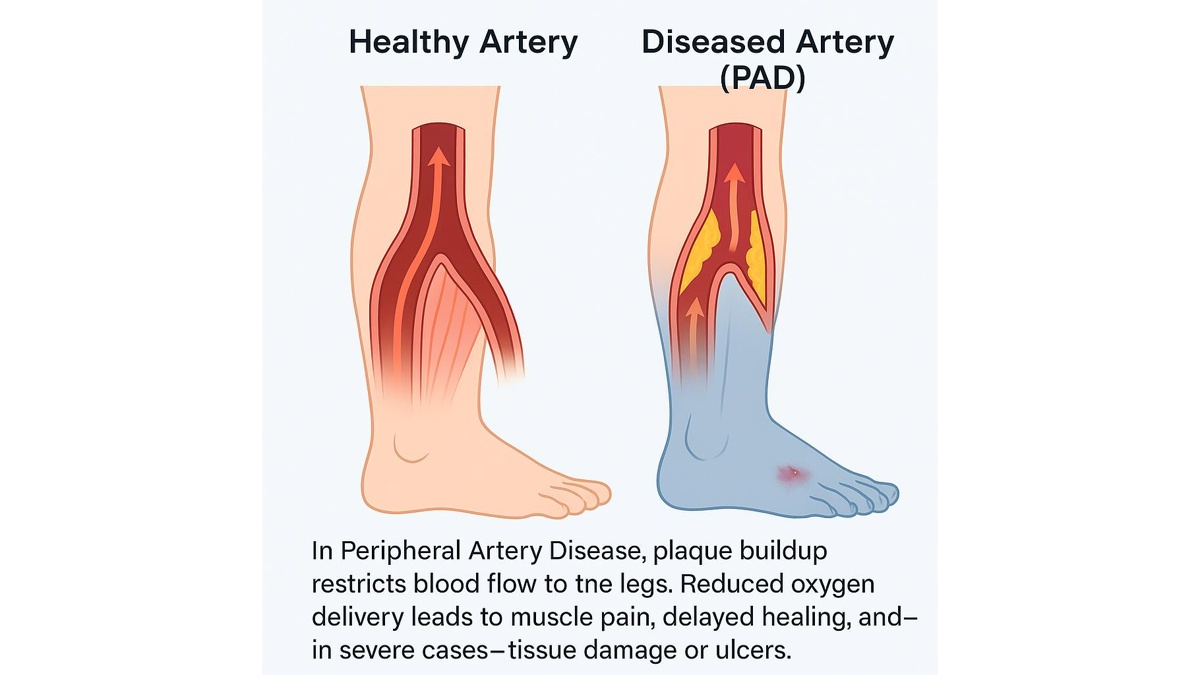
Peripheral Artery Disease (PAD) is a serious yet often overlooked condition affecting millions of people worldwide, including many in Virginia. When blood vessels in the legs become narrowed or blocked, oxygen-rich blood struggles to reach muscles and tissues. Over time, this lack of circulation causes pain, slows healing, and increases the risk of severe complications such as ulcers, infections, or even amputation.
Understanding Peripheral Artery Disease – its causes, early warning signs, and treatment options is essential for preserving mobility and quality of life. Fortunately, modern vascular medicine offers effective diagnostic tools and minimally invasive treatments, available at specialized centers such as Shenandoah Valley Surgical Associates (SVSA) in Fishersville, VA.
What Is Peripheral Artery Disease and How It Develops
Peripheral Artery Disease is a manifestation of atherosclerosis, the gradual buildup of fatty deposits (plaque) inside the arteries. Over time, these deposits harden and narrow the arterial walls, restricting blood flow to the limbs – most commonly to the legs and feet.
While Peripheral Artery Disease primarily affects the lower extremities, it signals a systemic vascular problem, meaning that atherosclerosis may also be developing in other arteries, such as those supplying the heart or brain. This is why PAD is not only a limb problem but a marker of cardiovascular disease that can increase the risk of heart attack and stroke.
Main Causes and Risk Factors
Several factors increase the likelihood of developing PAD:
- Smoking – the single strongest risk factor. Nicotine damages the inner lining of blood vessels, accelerates plaque buildup, and narrows arteries.
- Diabetes mellitus – chronically high blood sugar damages small and large blood vessels, leading to circulation issues.
- High blood pressure (hypertension) — puts continuous stress on arterial walls.
- High cholesterol – promotes fatty plaque accumulation in vessel walls.
- Age and gender – risk increases after age 50 and is slightly higher in men.
- Sedentary lifestyle and obesity – reduced physical activity worsens circulation and contributes to other risk factors.
Although PAD develops gradually, lifestyle choices play a significant role in both its prevention and progression. Quitting smoking, staying active, and controlling blood sugar and cholesterol are essential first steps.
The Role of Microcirculation and Inflammation
Recent studies emphasize the importance of inflammation and microvascular health. Chronic inflammation in the vessel walls attracts immune cells that further damage the endothelium (the inner arterial lining). This process not only accelerates plaque buildup but also makes plaques unstable, leading to sudden blockages.
Therefore, Peripheral Artery Disease is both a mechanical and inflammatory disease, which is why treatment often targets both the blockage itself and the underlying metabolic and inflammatory conditions.
Early Symptoms Peripheral Artery Disease and Typical Patient Complaints
The most common early sign of PAD is intermittent claudication — pain, cramping, or fatigue in the legs that appears during walking or exercise and disappears with rest. Patients often describe it as “tightness” or “aching” in the calves, thighs, or buttocks.
However, early PAD can be subtle. Many people attribute these symptoms to aging, joint problems, or muscle fatigue, delaying diagnosis until the disease becomes advanced.
Typical Peripheral Artery Disease Symptoms in the Legs
- Leg pain during walking or climbing stairs that improves after a few minutes of rest.
- Coldness or numbness in one or both feet.
- Pale or bluish skin tone on the legs or feet.
- Slow-healing sores or ulcers on the toes, feet, or legs.
- Weak pulse in the lower extremities when examined by a physician.
- Shiny skin, hair loss, or thickened toenails due to reduced circulation.
When PAD reaches advanced stages, pain may occur even at rest, especially at night when the legs are elevated. This condition — known as critical limb ischemia – requires urgent vascular evaluation and often intervention.
When to See a Vascular Specialist
If you experience leg discomfort that limits your walking distance, wounds that don’t heal, or notice color changes in your skin, you should not ignore these signs. Early evaluation by a vascular specialist is crucial.
In Fishersville, VA, patients can undergo comprehensive PAD screening at Shenandoah Valley Surgical Associates, where specialists perform advanced testing such as Ankle-Brachial Index (ABI) and vascular ultrasound to assess blood flow and detect blockages before complications develop.
Diagnostic Methods (Peripheral Artery Disease Testing at SVSA: ABI, Ultrasound, Angiography)
Diagnosing Peripheral Artery Disease (PAD) requires a careful combination of clinical evaluation and advanced vascular testing. Because PAD symptoms can resemble joint or nerve problems, accurate diagnosis ensures that treatment targets the real cause — restricted blood flow to the legs.
At Shenandoah Valley Surgical Associates (SVSA) in Fishersville, Virginia, vascular specialists provide a full spectrum of non-invasive diagnostic options to identify blockages early and evaluate circulation precisely. The most common diagnostic methods include the Ankle-Brachial Index (ABI) test, Duplex Ultrasound, and Angiography.
Ankle-Brachial Index (ABI)
The ABI test measures the difference between blood pressure in the ankle and the arm. If the ankle pressure is significantly lower, it indicates a narrowing of the arteries in the legs.
An ABI result of 1.0 or higher is normal, while a reading below 0.9 suggests the presence of PAD. This simple, painless test takes only a few minutes and often serves as the first-line screening tool for anyone experiencing leg discomfort or fatigue while walking.
Duplex (Doppler) Ultrasound
If the ABI suggests reduced circulation, a vascular ultrasound provides a visual map of blood flow. Using high-frequency sound waves, this test detects where arteries are narrowed or blocked and evaluates how severe the restriction is.
Ultrasound imaging is non-invasive, does not involve radiation, and can be repeated safely for follow-up monitoring. It is particularly useful for determining whether a patient might benefit from medical therapy or an interventional procedure.
CT and MR Angiography
When more detailed images are needed, CT angiography (CTA) or MR angiography (MRA) may be performed. These imaging techniques produce high-resolution, three-dimensional views of the arteries.
CTA uses contrast dye and X-rays to outline the blood vessels, while MRA uses magnetic fields — an alternative for patients who cannot tolerate iodine-based contrast. Both methods are invaluable for planning interventions such as angioplasty or bypass surgery.
Digital Subtraction Angiography (DSA)
In advanced cases or before treatment, physicians may perform catheter-based angiography. A thin catheter is guided into the artery, and contrast dye highlights the vessels under X-ray imaging.
This procedure provides unmatched precision and can transition seamlessly into treatment — if a blockage is found, the vascular specialist can immediately perform angioplasty or stent placement.
Modern Treatment Options – From Medications to Angioplasty
Treatment for Peripheral Artery Disease focuses on restoring circulation, relieving pain, and preventing complications like ulcers or tissue loss. The exact plan depends on disease severity and the patient’s overall health.
At SVSA in Fishersville, the care approach is comprehensive and personalized, combining lifestyle management, medication, and, when necessary, minimally invasive procedures.
Lifestyle Modification
Addressing underlying risk factors is the cornerstone of PAD management. Quitting smoking, maintaining a balanced diet, and engaging in regular physical activity can significantly improve blood flow and slow disease progression.
Even simple daily walking routines, supervised by a vascular specialist, help develop collateral circulation — small blood vessels that naturally bypass blocked arteries.
Medication
For many patients, medications are the next step. Antiplatelet drugs such as aspirin or clopidogrel help prevent blood clots, while statins reduce cholesterol and stabilize arterial plaque. Cilostazol may improve walking distance by enhancing blood flow to leg muscles.
Blood pressure and blood sugar control are also essential, particularly for patients with diabetes or hypertension, since uncontrolled levels accelerate vascular damage.
Endovascular Procedures
When medication alone is not enough, modern endovascular treatments can reopen blocked arteries through small punctures rather than open surgery. The most common procedures include:
- Angioplasty – inflating a small balloon to widen the artery.
- Stent placement – inserting a mesh tube to keep the vessel open.
- Atherectomy – mechanically removing plaque from the arterial wall.
These interventions are performed under local anesthesia, allowing for quick recovery and minimal discomfort. Most patients return home the same day.
Surgical Bypass
For long or complex blockages, bypass surgery may be required. A vein or synthetic graft is used to reroute blood around the diseased segment of the artery. Although it is a more invasive procedure, it provides durable long-term results and helps preserve limb function in severe cases.
Stages of PAD and Recommended Management
| Stage of PAD | Primary Symptoms | Recommended Approach |
|---|---|---|
| I (Early) | Pain while walking more than 200 meters | ABI testing, lifestyle modification |
| II (Moderate) | Pain at 100–200 meters | Vascular ultrasound, initiate medication |
| III (Critical) | Rest pain, non-healing ulcers | Angioplasty, stent placement, or bypass surgery |
Rehabilitation and Follow-up
Recovery after Peripheral Artery Disease treatment focuses on maintaining healthy circulation and preventing recurrence. Regular follow-up visits, including periodic ABI testing and vascular imaging, allow physicians to monitor improvements and detect any new blockages early.
Rehabilitation typically includes:
- Gradual walking programs designed to rebuild endurance.
- Ongoing control of risk factors such as cholesterol, blood pressure, and diabetes.
- Continued use of prescribed medications and smoking cessation support.
At SVSA, each patient receives a tailored rehabilitation plan to help restore mobility, reduce discomfort, and maintain long-term vascular health.
Prevention and Recovery After Treatment
Preventing Peripheral Artery Disease (PAD) or avoiding its recurrence after treatment requires a lifelong commitment to vascular health. Even after successful angioplasty or surgery, atherosclerosis can continue to progress unless the underlying risk factors are managed.
Healthy Lifestyle as the Best Medicine
The cornerstone of PAD prevention is maintaining healthy arteries through lifestyle changes. Quitting smoking is the single most effective action a patient can take – tobacco directly damages blood vessels and accelerates plaque buildup.
A diet rich in fresh fruits, vegetables, whole grains, and omega-3 fatty acids helps control cholesterol levels and reduces inflammation. Limiting saturated fats, salt, and processed foods further protects the vascular system.
Regular exercise, particularly walking programs, remains one of the most proven methods for improving leg circulation. Walking encourages the growth of collateral arteries, which naturally bypass blockages and improve blood delivery to muscles.
Managing Chronic Conditions
People with diabetes, high blood pressure, or high cholesterol are at greater risk for Peripheral Artery Disease and should keep these conditions under strict control. This includes regular check-ups, medication adherence, and home monitoring. Maintaining HbA1c below 7%, LDL cholesterol below 70 mg/dL, and blood pressure below 130/80 mmHg significantly lowers the risk of vascular complications.
Post-Treatment Rehabilitation
After angioplasty, stent placement, or bypass surgery, rehabilitation focuses on restoring mobility and confidence. Patients are encouraged to start walking as soon as possible, under guidance from their vascular specialist.
A structured supervised exercise program, offered at centers such as Shenandoah Valley Surgical Associates (SVSA), helps patients gradually increase endurance and improve circulation. Wound care and proper foot hygiene are also critical, especially for diabetic patients.
Follow-up imaging — including periodic ABI tests or vascular ultrasounds — ensures that blood flow remains optimal and that any new narrowing is detected early.
FAQ: Common Questions About Peripheral Artery Disease
How can I recognize Peripheral Artery Disease at an early stage?
Early PAD may cause mild pain, fatigue, or cramping in the calves after walking. The discomfort goes away with rest. Some people notice cold or pale feet, slow-healing wounds, or decreased hair growth on the legs. If you experience these symptoms, it’s best to schedule a PAD screening in Fishersville, VA, to catch the disease before it worsens.
Can Peripheral Artery Disease be treated without surgery?
Yes. In many cases, PAD can be managed with lifestyle changes, exercise, and medication. Quitting smoking, walking regularly, and taking prescribed drugs to control cholesterol and blood pressure can significantly improve symptoms. However, if circulation becomes critically reduced, a minimally invasive procedure such as angioplasty may be necessary to restore proper blood flow.
What is an ABI test and why is it important?
The Ankle-Brachial Index (ABI) compares the blood pressure in your ankle with that in your arm. It’s a simple, painless test that shows whether your leg arteries are narrowed. An ABI test is one of the best screening tools to detect PAD early especially for smokers, diabetics, or people over 50.
Do exercises really help with Peripheral Artery Disease?
Absolutely. Walking is medicine for PAD. Regular walking sessions improve muscle efficiency and stimulate the formation of new, small blood vessels that compensate for blocked arteries. Over time, patients can walk farther with less pain. Many vascular clinics, including SVSA, offer supervised exercise programs designed specifically for PAD recovery.
Can Peripheral Artery Disease lead to amputation?
If untreated, severe PAD can cause ulcers, infections, and tissue death (gangrene), sometimes leading to amputation. Fortunately, early diagnosis and proper treatment can almost always prevent this outcome. With modern therapies such as angioplasty, stenting, and effective wound care, most patients maintain full mobility and avoid limb loss.
Take Action – Don’t Wait for Pain
PAD screening often develops silently, and by the time leg pain or wounds appear, circulation may already be severely reduced. The good news is that early screening saves limbs and lives.
Author:
Dr. Jacek J. Paszkowiak, MD, FACS